Understanding the Link Between Sleep and Diabetes
Sleep and diabetes are deeply interconnected. When you sleep well, your body repairs itself, balances hormones, and keeps blood sugar stable. But poor sleep disrupts these processes, leading to insulin resistance, sugar spikes, and stronger cravings for unhealthy foods.
How Does Sleep Affect Diabetes?
When patients ask me, “How does sleep affect diabetes?” I explain that sleep is not just about rest—it is an active repair phase for the body. During deep sleep, insulin sensitivity improves, glucose uptake by cells is enhanced, and the body’s metabolic rhythm stays balanced. But when sleep is disrupted, the opposite occurs: insulin resistance increases, glucose levels spike, and cravings for high-carb foods rise. This explains why the sleep and diabetes connection is so powerful.
Beyond this, poor sleep has both direct and indirect effects on blood sugar control.
Direct and Indirect Effects of Poor Sleep on Diabetes
Direct Effects – Hormonal and Physiological Changes
Poor sleep immediately disrupts the body’s hormonal balance and glucose regulation, which explains the strong connection between sleep and diabetes:
- Insulin Resistance Increases: Sleep loss reduces insulin sensitivity in muscle and fat cells, meaning glucose stays in the bloodstream instead of being absorbed.
- Cortisol Elevation: Lack of deep sleep keeps cortisol levels high at night. This “stress hormone” directly raises blood sugar by stimulating the liver to produce glucose.
- Growth Hormone Suppression: Deep sleep normally triggers growth hormone release, which supports fat burning and tissue repair. Interrupted sleep lowers growth hormone, impairing fat metabolism and making weight loss harder.
- Leptin and Ghrelin Dysregulation: Sleep deprivation decreases leptin (satiety hormone) and increases ghrelin (hunger hormone), directly raising appetite for high-carb foods.
- Sympathetic Nervous System Overdrive: Poor sleep activates the “fight or flight” system, leading to higher nighttime heart rate, blood pressure, and glucose release.
These direct hormonal changes explain why even a single bad night of sleep can result in higher fasting sugars the next morning.
Indirect Effects – Lifestyle and Behavioral Consequences
Poor sleep doesn’t just affect hormones; it also changes daily behavior and lifestyle in ways that indirectly worsen diabetes control. That’s why understanding the link between sleep and diabetes is so important for patients trying to maintain balanced glucose levels:
- Daytime Fatigue: Sleep-deprived patients often feel exhausted, reducing their motivation for physical activity. Lower movement means muscles burn less glucose, worsening insulin resistance.
- Reduced Willpower and Poor Food Choices: Tired brains crave quick energy. Patients often reach for sugary snacks, bread, or fried foods, which spike blood sugar further.
- Increased Caffeine and Stimulant Intake: To fight fatigue, patients consume more coffee, tea, or even sugary energy drinks, which can delay sleep at night and perpetuate the cycle.
- Stress and Irritability: Lack of sleep increases emotional stress, which triggers more cortisol release. Patients also report irritability and mood swings, leading to emotional eating.
- Disrupted Meal Timing: Fatigue often leads to late-night snacking, skipped breakfasts, or irregular meal schedules, all of which destabilize blood sugar levels.
- Weakened Immune System: Sleep deprivation lowers immune function, making diabetics more prone to infections—each infection further raising blood glucose.
Sleep Deprivation and Diabetes Risk
Missing out on quality sleep doesn’t just make you feel tired the next day—it sets off a chain reaction inside the body. Research shows that even a few nights of poor sleep can alter how your body processes glucose and responds to insulin. Over the long term, this ongoing disruption can significantly raise the risk of type 2 diabetes. This strong link between sleep and diabetes highlights why maintaining good rest is just as important as diet and exercise.
Can Poor Sleep Cause Diabetes?
Many patients wonder, “Can poor sleep cause diabetes?” The evidence suggests that chronic sleep deprivation increases the risk of developing type 2 diabetes. Inadequate sleep triggers insulin resistance, reduces glucose tolerance, and disrupts appetite-regulating hormones like leptin and ghrelin. Over time, these changes contribute to obesity and diabetes onset. Understanding the connection between sleep and diabetes can help individuals take proactive steps toward healthier sleep habits and better long-term health.
Sleep Deprivation and Insulin Resistance
Studies show that even a few nights of restricted sleep can lead to measurable insulin resistance. This means glucose cannot enter cells effectively, leaving more sugar circulating in the blood. Repeated cycles of poor sleep and elevated glucose create a vicious loop—worsening both sleep and diabetes management.
Sleep Disorders Common in Diabetes
Diabetes Sleep Disorders: Sleep Apnea, Restless Leg Syndrome, and More
Diabetes is often associated with several sleep disorders:
- Obstructive Sleep Apnea (OSA): Characterized by interrupted breathing at night, common in overweight diabetics.
- Restless Leg Syndrome (RLS): A neurological condition that disrupts sleep and increases fatigue.
- Insomnia: Difficulty falling or staying asleep, often linked to stress and high glucose levels.
The term diabetes sleep disorders highlights how interconnected these problems are. Poorly managed diabetes worsens these conditions, and in return, these disorders worsen blood sugar regulation.
Identifying Symptoms and When to See a Specialist
Symptoms to watch for include: loud snoring, frequent nighttime urination, morning fatigue, headaches, or unexplained spikes in fasting glucose. In such cases, a sleep study or consultation with a sleep specialist is recommended.
Physiological Mechanisms: Sleep, Hormones, and Blood Glucose
The relationship between sleep and diabetes is largely driven by hormonal shifts that occur overnight. Deep sleep acts as a critical window where hormones like insulin, cortisol, and growth hormone work together to regulate metabolism, repair tissues, and maintain stable glucose levels. When this cycle is disturbed, the entire balance of sugar control is affected.
Cortisol, Growth Hormone, and Insulin Interplay During Sleep
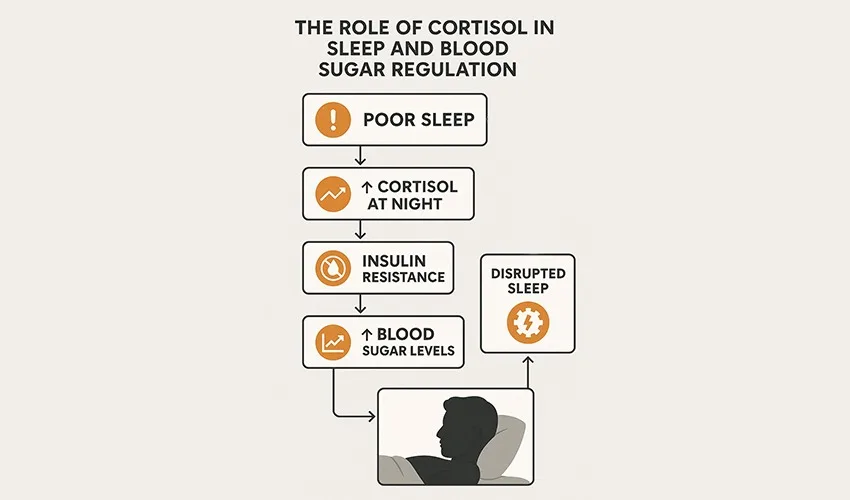
During deep sleep, growth hormone is released, which promotes fat metabolism and tissue repair. At the same time, insulin sensitivity improves, lowering nighttime glucose levels. When sleep is interrupted, growth hormone secretion drops, cortisol rises, and insulin resistance increases—leading to high morning blood sugars. This shows why the interplay between sleep and diabetes cannot be ignored in long-term health management.
Impact of Interrupted Sleep on Blood Glucose Levels
Interrupted or fragmented sleep prevents the body from entering deep restorative phases. This keeps glucose levels elevated overnight and raises HbA1c over time. Patients often notice that after nights of poor sleep, their blood sugar readings are consistently higher, reinforcing how strongly sleep affects blood glucose.
Improving Sleep for Better Diabetes Management
Better sleep isn’t just about feeling refreshed—it is a key part of blood sugar control. By focusing on healthy sleep habits, people with diabetes can reduce insulin resistance, lower stress hormones, and improve their overall metabolic balance. Small, consistent changes in the way you sleep can make a big difference in long-term diabetes management.
Best Sleep Habits for Diabetes
Establishing a Consistent Sleep Schedule
Going to bed and waking up at the same time every day—even on weekends—helps regulate circadian rhythms. This is one of the best sleep habits for diabetes, ensuring stable cortisol and insulin levels.
Optimizing Your Sleep Environment
A cool, dark, and quiet bedroom supports melatonin release. Avoid heavy carb-rich meals late at night, as they destabilize blood sugar and delay deep sleep.
Pre-Bedtime Routines that Promote Blood Sugar Balance
Simple habits like herbal teas, reading, or meditation before bed reduce stress and stabilize blood sugar. At Redial Clinic, we often recommend light stretching or breathing exercises as part of a sleep diabetes management protocol.
Lifestyle Strategies to Enhance Sleep Quality
Healthy sleep doesn’t happen by chance—it’s shaped by daily choices. The food you eat, how you manage stress, when you exercise, and even your bedtime routine all influence the depth and quality of your sleep.
Nutrition and Timing of Meals
Eating balanced low-carb dinners, rich in protein and healthy fats, prevents overnight blood sugar spikes. Avoiding caffeine and late-night snacks is key.
Exercise, Stress Reduction, and Mindfulness
Strength training in the evening helps improve insulin sensitivity and enhances deep sleep cycles. Stress management, through journaling or mindfulness, reduces cortisol levels.
Limiting Stimulants and Screen Time Before Bed
Blue light from screens delays melatonin secretion. Patients with diabetes should avoid late-night phone scrolling and instead practice a calming pre-bed routine.
Monitoring and Tracking Sleep in Diabetes Care
Devices and Apps for Sleep and Blood Sugar Tracking
Wearable devices like Fitbit or Apple Watch can track sleep duration, deep sleep, and HRV (heart rate variability). Combined with continuous glucose monitors (CGMs), they reveal real-time insights into the sleep and diabetes connection.
Integrating Sleep Data into Your Diabetes Management Plan
At Redial Clinic, we encourage patients to log sleep duration along with glucose readings. This helps identify patterns—like higher fasting sugars after poor sleep nights—and adjust diet, exercise, and bedtime routines accordingly.
When to Seek Professional Help
If sleep problems persist despite lifestyle adjustments, it’s crucial to seek medical evaluation. Sleep apnea, in particular, requires early detection and treatment, as it dramatically worsens diabetes outcomes.
What Sleep Strategies Does Redial Clinic Recommend for People with Diabetes?
At Redial Clinic, our approach includes:
- Structured bedtime routines tailored to individual patients.
- Dietary timing adjustments to prevent nighttime glucose fluctuations.
- Breathing techniques and stress management tools to reduce cortisol.
- Integration of sleep data into personalized diabetes reversal plans.
FAQs: Sleep and Diabetes
1) How does poor sleep quality impact blood sugar levels in people with diabetes?
Poor sleep raises cortisol and sympathetic activity, which increases hepatic glucose output and reduces insulin sensitivity. This leads to higher fasting sugars and unstable post-meal control.
2) Can sleep deprivation increase the risk of developing type 2 diabetes?
Yes. Chronic sleep deprivation triggers insulin resistance, appetite dysregulation, and obesity—all key drivers of type 2 diabetes.
3) What are the most common sleep disorders associated with diabetes?
- Sleep Apnea (interrupted breathing, snoring, fatigue)
- Restless Legs Syndrome (uncontrollable urge to move legs)
- Insomnia (difficulty falling or staying asleep)
4) Which hormones affected by sleep play a role in glucose metabolism?
- Insulin: sensitivity improves with good sleep.
- Cortisol: elevated with poor sleep, raising glucose.
- Growth Hormone: released in deep sleep, supports metabolism.
- Leptin & Ghrelin: control hunger; disrupted by poor sleep.
5) What practical strategies can I use to improve sleep for better diabetes management?
- Sleep/wake at the same time daily.
- Avoid late high-carb meals.
- Create calming pre-bed routines.
- Limit caffeine & blue light in evenings.
- Keep the bedroom cool, dark, and quiet.
6) How many hours of sleep should people with diabetes aim for?
7–9 hours of consistent, quality sleep is ideal.
7) Is it normal for fasting glucose to be higher after a bad night’s sleep?
Yes—elevated cortisol and sympathetic activation cause morning spikes.
8) Will treating sleep apnea improve blood sugar?
Yes. Sleep apnea treatment (e.g., weight loss) improves glucose control and energy.
9) Does melatonin help people with diabetes sleep better?
It may help with sleep onset, but should be used under medical guidance.
10) What’s the best time to exercise to support sleep and glucose control?
Afternoon or early evening strength training works best; avoid vigorous exercise right before bed.
11) Should I avoid late-night snacks?
Yes, especially carb-heavy snacks. If needed, choose small protein-fat combos (e.g., Greek yogurt, nuts).
12) Do naps affect nighttime sleep and blood sugar?
Short early-afternoon naps (10–20 min) are fine; long or late naps may harm sleep quality.
13) Can alcohol help me sleep?
No. Alcohol fragments sleep and destabilizes glucose levels.
14) How do I use wearables/CGM to improve my sleep–glucose patterns?
Overlay sleep duration with CGM data to identify triggers of poor sleep and high glucose.
15) I follow intermittent fasting—any sleep tips?
Keep feeding windows earlier, and ensure last meals include protein + healthy fats to avoid late hunger.
Conclusion and Key Takeaways
- The sleep and diabetes connection is undeniable—poor sleep worsens insulin resistance and raises glucose levels.
- Can poor sleep cause diabetes? Yes, sleep deprivation contributes to type 2 diabetes risk.
- Common diabetes sleep disorders like sleep apnea worsen blood sugar control.
- Hormones such as cortisol, insulin, and growth hormone play key roles in how sleep affects blood glucose.
- Adopting the best sleep habits for diabetes—consistent schedules, reduced stress, and optimized sleep environments—can transform blood sugar management.
- Ultimately, improving sleep for diabetes is just as important as diet and exercise.
Final Verdict
At Redial Clinic, Green Park, Delhi, we firmly believe that sleep is medicine for diabetes reversal. By prioritizing sleep quality alongside nutrition and strength training, our patients have achieved sustainable blood sugar control without dependency on medication. If you’re struggling with restless nights and unstable sugars, it’s time to take sleep seriously. With the right guidance, you can regain balance, energy, and control over your diabetes.
References
| No. | Source | Key Findings |
|---|---|---|
| 1 | American Diabetes Association – Sleep and Diabetes | Poor sleep increases insulin resistance and worsens glycemic control. |
| 2 | Harvard School of Public Health – Sleep & Obesity Studies | Sleep deprivation alters appetite hormones, increasing risk of obesity and diabetes. |
| 3 | National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) | Sleep apnea and restless leg syndrome are common in diabetes patients. |