Low-Carb Diet vs. Low-Fat Diet for Diabetes: Which One Really Works for Blood Sugar Control
Low-Carb Diet vs. Low-Fat Diet for Diabetes — this guide explains why carbohydrate restriction improves insulin resistance, stabilizes blood sugar, and supports sustainable weight loss.
Introduction: The Long-Running Diet Debate
For decades, standard diabetic nutrition guidelines focused on reducing dietary fat.
Patients were often told to eat:
- Chapati or brown rice instead of white rice
- Dal, lentils, sprouts as main proteins
- Minimal oil, butter, or desi ghee
The thinking was simple: “less fat = fewer calories = better sugar and weight control.”
But as type 2 diabetes and obesity continued to rise, it became clear that this low-fat approach was not solving the problem.
Patients still struggled with:
- High HbA1c despite calorie restriction
- Fatigue, cravings, and frequent hunger
- Progressive need for more medications
Today, large-scale studies and clinical practice — including our own experience at Redial Clinic — show that carbohydrates, not fats, drive blood sugar spikes and insulin resistance. Learn how we implement this in our Diabetes Reversal and Obesity Reversal programs.
Low-Carb Diet vs. Low-Fat Diet for Diabetes: Understanding the Root Problem
Understanding the Root Problem: Insulin Resistance
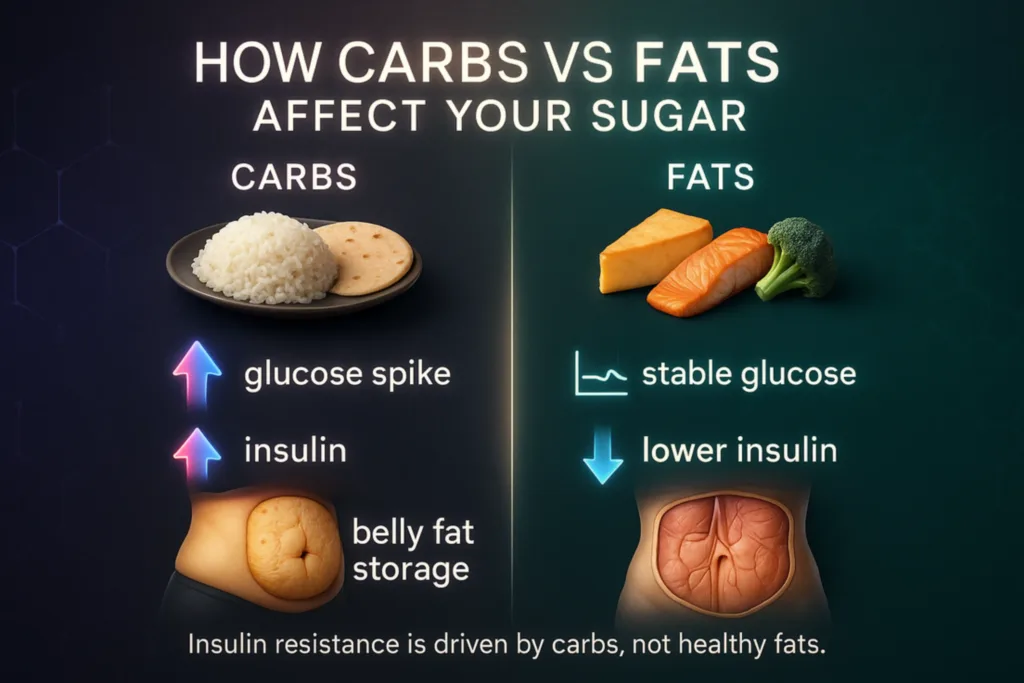
Type 2 diabetes is fundamentally a condition of carbohydrate intolerance.
How it develops:
- Carbohydrate intake → glucose spike: Foods such as rice, roti, bread, oats, or even millets are broken down into glucose.
- Insulin response: The pancreas releases insulin to move glucose into cells for energy.
- Resistance sets in: Chronically high insulin and glucose make cells less responsive.
- Cycle of disease: More insulin is secreted → more fat storage (especially in liver and belly) → worsening insulin resistance.
The Low-Fat Diet: Why It Often Fails in Diabetes
A conventional low-fat diabetic diet in India typically includes:
- 6–8 chapatis or bowls of brown rice/millets daily
- Pulses and legumes as primary protein
- Less than 20 g/day of ghee or oil
- Low-fat curd, skim milk, “diet snacks”
While this sounds “light and healthy,” it has several pitfalls.
High Glycemic Load
Whole grains and lentils still break down into glucose and raise post-meal sugars.
Persistent Insulin Demand
Continuous carb intake keeps insulin levels high → promotes fat storage → worsens resistance.
Energy Fluctuations & Cravings
Carb-heavy meals lead to sugar spikes followed by crashes, driving hunger and overeating.
Slow or Stalled Weight Loss
High insulin prevents efficient fat burning, making it harder to lose weight even with calorie restriction.
Case Study – Before Low-Carb:
A 52-year-old woman came to Redial Clinic with HbA1c 8.0% after a year of a conventional low-fat, calorie-restricted diet.
She felt constantly hungry and tired.
After switching to a supervised low-carb, high-protein, healthy-fat plan, her HbA1c dropped to 6.4% in 4 months, hunger reduced, and energy improved.
The Low-Carb Approach: How It Works
At Redial Clinic, a typical therapeutic low-carb plan provides:
- Carbohydrates: 15–20% of calories
- Protein: 25–30% of calories
- Healthy fats: 50–60% of calories
Core Food Components
- Proteins: paneer, tofu, eggs, chicken, fish (esp. Rohu, Salmon), mutton, goat liver
- Low-starch vegetables: lauki, tinda, turai, cabbage, cauliflower, broccoli, cucumber, spinach, zucchini
- Healthy fats: desi ghee, white makkhan, virgin coconut oil, extra virgin olive oil
We personalize these within Diabetes Reversal, and when needed, align with Hypertension Reversal and PCOS Management for comprehensive metabolic care.
How Low-Carb Diet vs. Low-Fat Diet for Diabetes Impacts Blood Sugar
This comparison matters clinically: the choice between a Low-Carb Diet vs. Low-Fat Diet for Diabetes directly influences post-meal glucose spikes, insulin demand, cravings, and long-term HbA1c trends.
Physiological Advantages of Low-Carb for Diabetes
Immediate Reduction in Glucose Load
Lower carb intake → less glucose absorbed → smaller post-meal spikes.
Less Insulin Required → Better Sensitivity
Pancreas gets a “rest”; cells become more responsive to insulin over time.
Sustained Energy and Satiety
Proteins and healthy fats digest slowly → more stable energy → fewer cravings.
Support for Fat Loss
Reduced insulin allows stored fat (esp. visceral fat and liver fat) to be used for energy.
Favorable Impact on Lipids
Research shows low-carb diets often lower triglycerides and raise HDL, improving cardiovascular risk.
Metabolic Outcome of Low-Carb vs. Low-Fat
| Outcome | Low-Fat Diet | Low-Carb Diet |
|---|---|---|
| Post-meal glucose | Often spikes sharply | Much lower, more stable |
| Insulin requirement | High | Lower |
| Weight loss | Slower, often plateaus | Faster, more sustainable |
| Hunger & cravings | Frequent | Lower, better satiety |
| Energy levels | Fluctuate with carb intake | More consistent throughout the day |
| Lipid profile | Mixed results | Improves HDL, lowers triglycerides |
The Redial Clinic Way
We never use a one-size-fits-all template.
Every patient’s plan is tailored to:
- Medical profile: diabetes duration, HbA1c, fatty liver, hypertension, cholesterol
- Body composition & activity: muscle mass, strength-training, daily routine
- Food preferences & culture: vegetarian, eggetarian, non-vegetarian
- Transition safety: gradual carb reduction to prevent keto-flu
- Outcome focus: reducing HbA1c, tapering medicines, supporting weight & metabolic health
Real Transformation – Redial Clinic Patient:
A 49-year-old male with diabetes, high cholesterol and fatty liver started our supervised low-carb program.
In 5 months, he lowered HbA1c from 7.8% to 5.9%, lost 10 kg, reduced belly fat, and could cut down on his diabetes medication.
These protocols are delivered through our Diabetes Reversal pathway and supported by Lifespan Extension where appropriate.
Addressing Common Myths
Myth: Low-Carb Harms the Heart
✅ Truth: Replacing refined carbs with natural fats such as desi ghee, white makkhan, virgin coconut oil, and extra virgin olive oil improves lipid profile.
Myth: Vegetarians Can’t Follow Low-Carb
✅ Truth: Vegetarian low-carb is very achievable with paneer, tofu, tempeh, Greek yogurt, and seasonal vegetables.
Myth: Low-Carb Is Just a Short-Term Fad
✅ Truth: Long-term studies show sustained improvements in blood sugar, weight, and cardiovascular markers.
Practical Tips for Patients Starting Low-Carb
- Replace roti/rice with more non-starchy vegetables and proteins like paneer/egg portions.
- Cook with real fats (desi ghee, white makkhan, virgin coconut or extra virgin olive oil); avoid refined seed oils.
- Include protein at every meal to keep muscles strong and hunger in check.
- Avoid processed “low-fat” or “sugar-free” snacks — many contain hidden carbs.
- Track blood sugars regularly as medication needs often reduce quickly on low-carb.
- Work with an experienced medical-nutrition team like Redial Clinic for safe and customized guidance.
Key Takeaways
- Low-fat diets focus on calories but leave insulin resistance unaddressed.
- Low-carb diets tackle the root cause of diabetes — excessive carbohydrate load and insulin demand.
- Evidence and real-world results show better HbA1c reduction, weight loss, lipid improvement, and patient satisfaction with low-carb.
Final Verdict
The debate around the Low-Carb Diet vs. Low-Fat Diet for Diabetes is settled by outcomes: low-carb, high-protein, healthy-fat nutrition is not a passing trend — it’s a science-based, root-cause approach that helps restore metabolic health in people with type 2 diabetes. At Redial Clinic, our experience with thousands of Indian patients shows that switching from a conventional low-fat plan to a carefully supervised low-carb program consistently improves blood-sugar control, reduces dependence on medications, and enhances quality of life. 📍 If you’re struggling despite “eating healthy,” it’s time to rethink your plate. Book your personalized consultation at Redial Clinic, Green Park, Delhi and learn how a properly designed low-carb approach can help you reverse diabetes naturally and sustainably. Start with our Diabetes Reversal program; related pathways include Obesity Reversal and Hypertension Reversal.
FAQs
Q. Is a low-carb diet safe for people with type 2 diabetes?
When medically supervised and properly formulated, low-carb is safe and often improves HbA1c, weight, triglycerides, and medication needs.
Q. Low-carb vs. low-fat — which is better for blood sugar control?
Evidence and clinical outcomes consistently show low-carb provides better post-meal glucose stability and insulin demand reduction than low-fat.
Q. Can vegetarians follow a low-carb plan?
Yes. Paneer, tofu, tempeh, eggs (if eggetarian), Greek yogurt, and seasonal low-starch vegetables make vegetarian low-carb very achievable.
Q. Will my medications need adjustment on low-carb?
Often yes. As blood sugars improve, medications may need tapering — always coordinate changes with your clinician.
Q. How many carbs per day count as “low-carb”?
Therapeutic ranges vary, but many plans start near 15–20% of calories from carbs and adjust to response and safety.
References
| No. | Source | Key Findings |
|---|---|---|
| 1 | Hallberg SJ et al., Diabetes Therapy, 2018 | Low-carb diet significantly lowered HbA1c and reduced need for medication compared with standard low-fat care. |
| 2 | Meng Y et al., Nutrients, 2017 | Meta-analysis: low-carb diets improved glycemic control and lipid profile in people with type 2 diabetes. |
| 3 | Feinman RD et al., Nutrition, 2015 | Carbohydrate restriction had the greatest impact on lowering post-prandial glucose and insulin demand. |
| 4 | Tay J et al., Annals of Internal Medicine, 2015 | Low-carb diet outperformed low-fat for glycemic control and cardiovascular risk factors in type 2 diabetes. |
| 5 | Virta Health Study, Frontiers in Endocrinology, 2019 | Patients on low-carb, high-fat nutrition maintained lower HbA1c and greater weight loss over 2 years. |
| 6 | NIH NIDDK – Type 2 Diabetes Overview | Outbound reference: Explains insulin resistance, carbohydrate metabolism, and lifestyle strategies relevant to diet-based blood sugar control. |