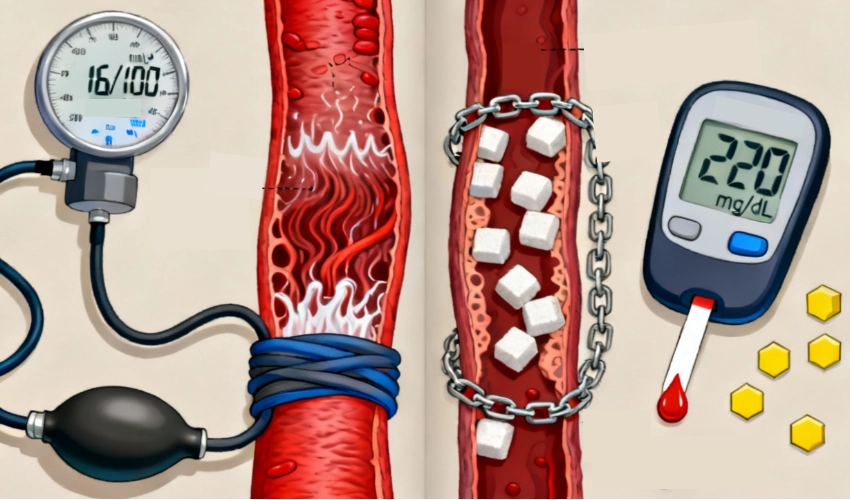
Hypertension & Diabetes often occur together — this guide explains the root metabolic link and how addressing insulin resistance can reverse both.
Introduction: A Deadly Duo on the Rise
Hypertension (high blood pressure) and type 2 diabetes often travel together. Studies show that up to 60–70% of people with type 2 diabetes also have hypertension, and this combination significantly increases the risk of heart disease, stroke, kidney damage, and even early death. While most people view these as two separate conditions—one affecting blood sugar, the other affecting blood pressure—they share a common root cause: insulin resistance. Understanding this link is crucial to break the cycle and reverse both conditions, not just manage them with lifelong medication.
At Redial Clinic, we address both conditions together via our integrated programs: Diabetes Reversal and Hypertension Reversal.
The Biology Behind the Link in Hypertension & Diabetes
1. Insulin Resistance as the Common Denominator
In healthy individuals, insulin helps cells absorb glucose for energy. In insulin resistance, cells become “deaf” to insulin. The body compensates by producing more insulin (hyperinsulinemia). This excess insulin:
- Promotes salt and water retention, leading to higher blood pressure.
- Stimulates the sympathetic nervous system, increasing heart rate and vessel constriction.
- Worsens weight gain—especially around the abdomen—further fueling both diabetes and hypertension.
Targeting insulin resistance through a structured lifestyle plan (see Obesity Reversal) is often the shortest path to improving both BP and glucose control.
2. Chronic Inflammation and Endothelial Dysfunction
Persistently high blood glucose damages the endothelium, the inner lining of blood vessels. Inflammation and oxidative stress reduce vessel flexibility, increasing vascular resistance—one of the hallmarks of hypertension. The same damaged blood vessels also reduce blood flow to insulin-sensitive tissues (like muscles), making glucose control even harder.
3. Renin–Angiotensin System (RAS) Overdrive
Insulin resistance activates the RAS, which constricts blood vessels and raises blood pressure. Over time, it also contributes to diabetic kidney disease, which further worsens hypertension.
Why Managing One Without the Other Fails

Traditional medical approaches often treat the two conditions separately:
- Antihypertensive drugs lower BP but don’t address insulin resistance.
- Antidiabetic drugs lower blood sugar but don’t directly reduce blood pressure.
The result: patients often end up on 3–5 medications, yet the underlying metabolic problem continues to worsen. At Redial Clinic, we emphasize root-cause reversal—by addressing insulin resistance, we often see improvements in both blood sugar and blood pressure within weeks. Explore our integrated care: Diabetes Reversal · Hypertension Reversal.
Lifestyle & Dietary Triggers That Fuel Both
- High-carbohydrate Indian staples (dal–chawal, rotis, poha, bread).
- Processed foods and snacks (biscuits, namkeen, breakfast cereals, “healthy” muesli).
- Sugary beverages and late-night eating.
- Sedentary lifestyle and chronic stress.
Clinical Insight: High-carb intake drives frequent insulin spikes; when insulin is chronically high, kidneys retain sodium—elevating blood pressure. For tailored nutrition, see our Diabetes Reversal and PCOS Management programs.
Breaking the Cycle: The Diabetes–Hypertension Reversal Approach
At Redial Clinic, our approach focuses on:
Low-Carb, High-Protein, Healthy Fat Diet
- Reduces insulin spikes → lowers both blood sugar and blood pressure.
- Emphasizes desi ghee, white makkhan, virgin coconut oil, extra virgin olive oil.
- Cuts out refined carbs, sugary snacks, and processed oils.
Weight & Visceral Fat Reduction
- Targeted strength training builds lean muscle and improves insulin sensitivity.
- Reduction in waist circumference often precedes blood pressure normalization.
Electrolyte Balance & Salt Re-education
- On well-formulated low-carb plans, moderate natural salt is often tolerated once insulin drops and kidneys excrete excess water.
Stress Management & Sleep Optimisation
- Lower cortisol improves both insulin sensitivity and vascular health.
Adjunct pathways that support outcomes: Lifespan Extension and Anti-Cancer Diet Support.
Case Study: Transforming Metabolic Health
Patient: Ramesh, 54 years; HbA1c 8.1%, BP 150/95 mmHg; on 2 antihypertensives & 2 antidiabetic drugs.
Approach: Low-carb, high-protein diet with healthy fats; strength training 3×/week; eliminated late-night carb snacks.
Outcome (in 4 months):
- HbA1c dropped to 6.2%.
- BP reduced to 125/80 mmHg; one BP medicine discontinued.
- Lost 9 kg; waist circumference reduced by 10 cm.
Insight: Addressing insulin resistance helped reverse both conditions with fewer medications. This reflects a root-cause strategy for Hypertension & Diabetes.
FAQs
Q1: Which comes first—diabetes or hypertension?
Either can appear first, but both share insulin resistance as a root cause. Treating the root improves outcomes for both.
Q2: Can reducing carbs really help blood pressure?
Yes. Lower insulin allows kidneys to excrete sodium and water more effectively, reducing BP naturally.
Q3: Should I stop my medications if I improve with lifestyle?
Never stop abruptly. Work with your doctor to taper medications as your health markers improve.
⭐ Final Verdict: Heal the Root, Not Just the Symptoms
Hypertension & Diabetes often appear as two separate diagnoses, but in reality, they are two symptoms of the same underlying problem—insulin resistance. Treating one while ignoring the other only manages the numbers; it doesn’t protect long-term health. At Redial Clinic, we focus on reversing the root metabolic dysfunction. By shifting patients to a low-carb, protein-rich, healthy-fat diet, improving muscle strength and activity, and guiding stress and sleep management, we’ve seen consistent transformations:
- Blood sugar levels stabilize naturally.
- Blood pressure often comes down within weeks.
- Medication needs decline, sometimes dramatically.
- Energy levels, waistline, and cardiovascular risk all improve together.
If you’re living with either hypertension, diabetes, or both, the answer isn’t just tighter control—it’s genuine reversal of insulin resistance. Start here: Diabetes Reversal · Hypertension Reversal · Obesity Reversal.
📚 References
| No. | Source | Key Findings |
|---|---|---|
| 1 | UK Prospective Diabetes Study (UKPDS) | ~60% of people with type 2 diabetes also had hypertension; dual presence increased cardiovascular risk 2–3×. |
| 2 | Circulation (AHA Journal), 2021 | Insulin resistance linked to increased sympathetic activity and vascular stiffness—key drivers of hypertension. |
| 3 | Diabetologia, 2020 | Weight loss and low-carb dietary patterns improved insulin sensitivity and reduced fasting glucose and systolic BP. |
| 4 | The Lancet Diabetes & Endocrinology, 2019 | Early lifestyle intervention can prevent or delay onset of both diabetes and hypertension in at-risk individuals. |